All About Age-related Macular Degeneration
Age-related macular degeneration (AMD) is one of the top causes of vision loss in people aged sixty and older. It is a disease that hampers your sharp, central vision. Central vision is pivotal to helping you see objects clearly and do tasks like driving and reading. AMD impairs your macula, the part of the eye that helps you see fine detail. It is not painful, but it kills the cells in the macula. It starts with blurred vision, but you gradually lose central sight.
Seeing crooked lines is one of the initial AMD signs. In this guide, we will discuss everything related to AMD in detail.
Types of AMD
Dry
People with dry AMD have drusen or yellow spots in the macula. Small drusen might not necessarily impair your vision, but as they grow in size and increase in number, they distort and dim your vision, especially as you read. Over time the condition worsens, and the light-sensitive cells in the macula get thinner and die eventually. If it is in the atrophic form, you will experience a blind spot in the center of the vision. Consequently, it worsens, and you lose central sight.
Wet
Blood vessels grow below the macula. These leak fluid and blood into the retina. So, when your vision is distorted, the straight lines look wavy. It might also lead to blind spots. At times, the blood vessels may bleed, leaving a scar and causing you to lose your central vision forever.
Typically, people with age-related macular degeneration have dry AMD. But, sometimes, the dry form might eventually result in wet AMD. Only 1 in 10 people with macular degeneration get wet AMD. When you have macular degeneration, you must see your eye doctor frequently and closely monitor your eyesight.
AMD symptoms
The AMD symptoms depend on the stage. It is a progressive disease, and there are three stages in dry AMD – early, intermediate, and late, meaning the symptoms aggravate or worsen over time.
In early AMD, you may not have any symptoms. Some people show no signs even in the intermediate stage, but others might have mild symptoms like difficulty seeing in low light and mild blurriness in the central vision. The presence of tiny yellow deposits or drusen in the retina is also one of the first signs of AMD, meaning one eye is at a greater risk of developing more severe AMD.
People see straight lines looking crooked or wavy when AMD progresses to the advanced stage. In addition, you might see a blurry area near the vision center. Sadly, the blurry region only advances over time, and you might also see blank spots and experience difficulty recognizing familiar faces. There will be more trouble seeing in the low light, and the colors will seem lighter than before. Hence, anytime you feel the straight lines look wavy, you must immediately see a doctor.
AMD causes
Unfortunately, there is no clarity on the specific cause of macular degeneration. However, the interplay between environmental factors and hereditary is tricky. Hence, the more scientists comprehend the mechanisms responsible for the macular cells to deteriorate, the higher the probability of discovering potential treatments to curtail the disease. Of course, the challenges are massive as several environmental factors are genes are linked to AMD. In addition, sun exposure and what you eat might also be responsible for AMD.
Risk factors
Some factors aggravate your risk of developing AMD. These include:
- Age
AMD is prevalent in people older than sixty years. - Cardiovascular diseases
People with a blood vessel or heart condition are susceptible to developing AMD. - Genetics and familial link
AMD has a hereditary component. Scientists even link some genes to these conditions.
Diagnosis
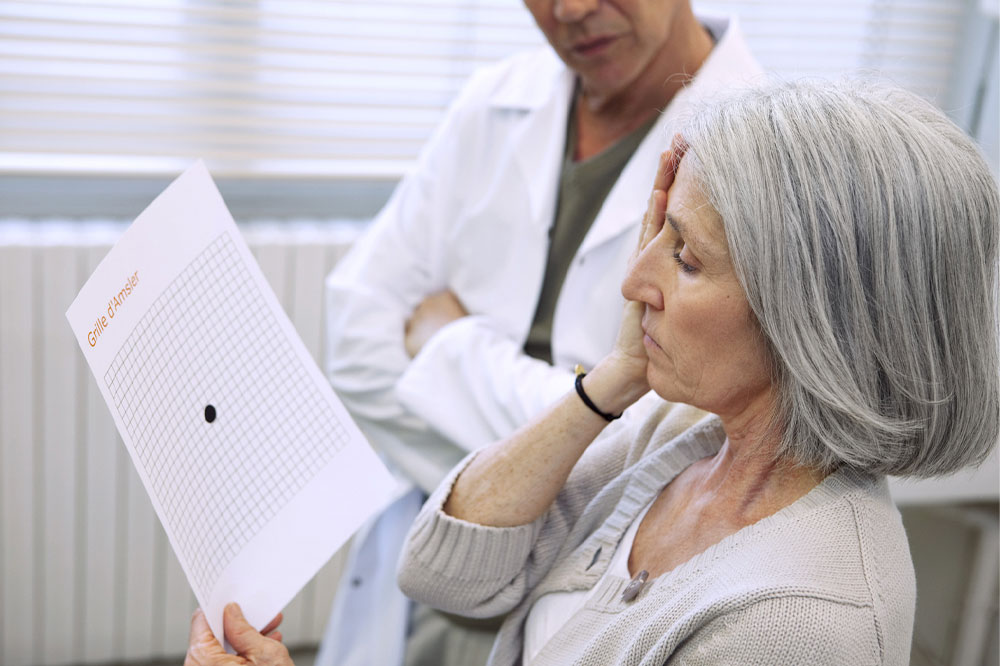
If you experience any of the above-stated signs, you must consult an optometry doctor immediately and get a comprehensive eye examination. This test can determine whether you have any eye-related condition or AMD. An optometry doctor might recommend a simple take-home screening test, Amsler Grid.
Sadly, you cannot restore the central vision lost from AMD. But, low-vision devices like microscopic and telescopic lenses can help maximize the existing sight.
Treatment options
As stated, there is no available cure for AMD. But, some treatments might prevent you from losing most of your vision or slow the disease progression. Some of the available options include:
- Anti-angiogenesis
These include bevacizumab (Avastin), aflibercept (Eylea), ranibizumab (Lucentis), pegaptanib (Macugen), and faricimab-svoa (Vabysmo). They help block blood vessel formation and any leaking from the vessels into the eye, a prevalent AMD cause. Studies show that people who chose anti-angiogenesis got back some of their lost vision, but you will have to get this treatment several times for concrete results. - Laser therapy
This therapy involves high-energy laser light to kill any abnormal blood vessels forming in the eye. - Photodynamic laser therapy
This therapy involves injecting a light-sensitive antidote, verteporfin (Visudyne), into your bloodstream. Visudyne gets absorbed by abnormal blood vessels. Following this, the eye expert will shine a laser into the eye, stimulating Visudyne to kill these blood vessels. - Low vision aids
Some devices have electronic systems or special lenses that help form a bigger image of the objects nearby, allowing people with AMD to make the most of their leftover vision.
Beyond this, researchers are also studying several newer therapies and treatments for macular degeneration, but they are experimental. These include: - Retinal translocation
This is a procedure to kill the abnormal blood vessels beneath the macula center. It helps reach where the laser beam cannot be used safely. It involves rotating the macula center away from the infected blood vessels to a healthier spot in the retina. Consequently, there is no further damage to the retina. Once done, the doctor employs a laser to cure the abnormal blood vessels. - Submacular surgery
It involves removing abnormal blood vessels.
Preventive measure
Some preventive measures can lower the risk of age-related macular degeneration and help you lead a healthier lifestyle. These include exercising as much as you can and eating nutrient-rich foods.





